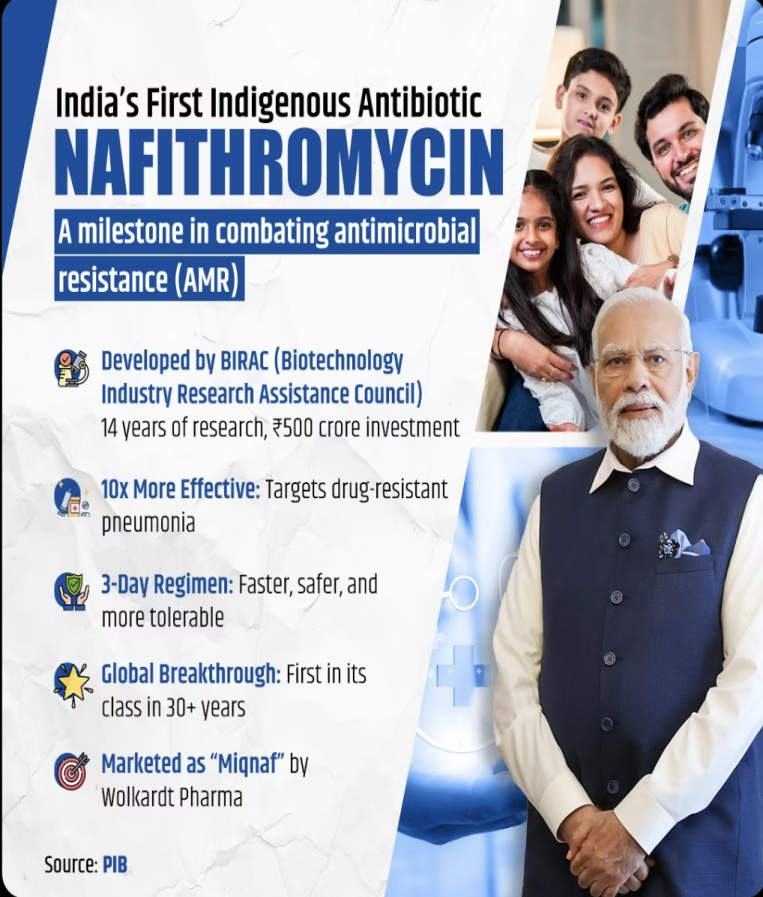
GOI launched Nafithromycin, India’s first indigenously developed antibiotic, addressing Antimicrobial Resistance and Community-Acquired Bacterial Pneumonia with high efficacy and safety, supported by BIRAC(Biotechnology Industry Research Assistance Council).
This is India’s first indigenously developed antibiotic designed to combat antimicrobial resistance (AMR). This development brings hope for treating drug-resistant pneumonia, which is responsible for over two million deaths globally each year.
Key Takeaways
1. Nafithromycin is designed for the treatment of Community-Acquired Bacterial Pneumonia (CABP), a serious illness caused by drug-resistant bacteria that affects vulnerable populations, including children, the elderly, and immunocompromised individuals such as patients with diabetes and cancer.
2. Nafithromycin is marketed as “Miqnaf” by the pharmaceutical company Wolkardt. It is 10 times more potent than Azithromycin, a safer, faster, and more tolerable solution for patients. Its outcome is good with just a three-day regimen as validated by clinical trials.
3. It has been developed with support from the Biotechnology Industry Research Assistance Council (BIRAC), which is a unit of the Department of Biotechnology.
4. Nafithromycin targets both typical and atypical pathogens, providing a strong solution in a time when no new antibiotics in this class have been developed globally for over thirty years. In addition to its effectiveness, Nafithromycin is known for its superior safety and tolerability.
The antibiotic has minimal gastrointestinal side effects, does not have significant drug interactions, and is not affected by food, making it a versatile option for patients.
Source: PIB, Indian Express
Pnuemonia
1. Pneumonia is a disease that affects the lungs. The lungs have small air sacs called alveoli, which fill with air when you breathe in.
When an individual has pneumonia, the alveoli are filled with pus and fluid, which makes breathing painful and limits oxygen intake.
2. In children, pneumonia is caused by a number of infectious agents, such as bacteria, viruses and fungi.
The most common cause of bacterial pneumonia in children is Streptococcus pneumoniae, followed by Haemophilus influenzae type b (Hib). The respiratory syncytial virus is the most common viral cause of pneumonia in children.
3. Pneumonia can spread in several ways. When a child inhales viruses and bacteria that are often present in their nose or throat, these microorganisms can infect the lungs.
Additionally, airborne droplets from a cough or sneeze can carry infectious agents. Pneumonia can also spread through the blood, especially during and shortly after childbirth.
Antimicrobial resistance (AMR) is one of the top global public health and development threats. It is estimated that bacterial AMR was directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths.- World Health Organisation
Antimicrobial resistance
Antimicrobial resistance (AMR) is a condition in which bacteria, viruses, fungi and parasites no longer respond to antimicrobial medicines, which include antibiotics, antivirals, antifungals and antiparasitics. As a result, infections become difficult or impossible to treat, increasing the risk of disease spread, severe illness, disability and death. It is the result of evolution of microbes in a situation where there is a misuse or overuse of antibiotics.
National Programme on AMR Containment: It was launched during the 12th Five Year Plan (2012-17). The main objectives of this program are:
📍Establish a laboratory-based antimicrobial resistance (AMR) surveillance system in the country to generate high-quality data on antimicrobial resistance.
📍Conduct surveillance of antimicrobial usage in different healthcare settings.
📍Strengthen infection control practices and promote the rational use of antimicrobials through antimicrobial stewardship activities.
📍 Raise awareness among healthcare providers and the community about antimicrobial resistance and the rational use of antimicrobials.
National Action Plan (NAP) on AMR: India was among the first countries to develop a comprehensive NAP on Antimicrobial Resistance in 2017. The plan focuses on a One Health approach, involving various stakeholder ministries and departments.